Recognizing Perioperative Tachycardia
Recognizing Perioperative Tachycardia
Blog Article
Perioperative tachycardia, a common occurrence during surgical procedures and the immediate following period, presents a issue for healthcare professionals. It refers to a rapid heart rate greater than a predetermined threshold, typically classified as 100 beats per minute or more. This condition can arise from a variety of factors, ranging from physiological stress, anxiety, pain, and underlying medical conditions. Understanding the causes and potential implications of perioperative tachycardia is crucial for providing optimal patient care.
Early identification and management are necessary to minimize complications. Healthcare providers should meticulously observe patients' heart rates during the perioperative period and implement appropriate interventions, such as medication administration, to restore hemodynamic stability.
Treating Postoperative Tachycardia: A Clinical Guide
Postoperative tachycardia, a frequently observed complication following surgery, can involve significant challenges for clinicians. This phenomenon is characterized by an elevated heart rate as well as typically remains elevated a prolonged period post-procedure.
Understanding the underlying mechanisms of postoperative tachycardia is crucial for developing effective management strategies. Various factors can contribute to this occurrence, including pain, anxiety, fluid shifts, and autonomic nerve system alteration.
Effective control of postoperative tachycardia requires a multimodal approach. Pharmacological often play a pivotal role, with options such as beta-blockers and calcium channel blockers utilized to regulate heart rate. Alongside medication therapy, non-pharmacological can be beneficial. These may include stress reduction techniques, optimization of pain management, and sufficient fluid administration.
The comprehensive assessment of the patient's clinical status, with consideration to their medical history, current medications, and postoperative course, is essential for personalizing the management plan. Close monitoring of vital signs, including heart rate, blood pressure, and oxygen saturation, is crucial to maintain patient safety and successfully manage postoperative tachycardia.
Perioperative Tachycardia: Causes and Considerations
Elevated heart rates during the perioperative period can manifest as a common physiological response to various factors. A myriad of contributors can give rise to this phenomenon, ranging from anesthetic agents and surgical stress to underlying medical conditions.
It's crucial for clinicians to accurately evaluate the root cause of perioperative heart rate elevation, as it can influence patient outcomes and inform management strategies. A comprehensive history should include a detailed review of the patient's anesthetic history, baseline vital signs, and current medications.
Additionally, neurological examination findings can provide valuable clues regarding potential underlying concerns.
Could Tachycardia After Surgery Normal? Exploring Common Causes
Following a surgical procedure, the patient's heart rate may sometimes increase. This accelerated heartbeat, known as tachycardia, can be a common occurrence in the postoperative period. That said, understanding the root causes of tachycardia after surgery is crucial for accurate diagnosis and treatment. Some typical culprits include pain, anxiety, dehydration, medications, and a drop in blood volume. In many cases, tachycardia resolves on its own as the body recovers.
However, if you are observing persistent or severe tachycardia after surgery, it's critical to consult with your healthcare provider immediately.
The Incidence and Impact of Perioperative Tachycardia
Perioperative tachycardia occurs in a significant proportion of patients undergoing surgical procedures. This condition, characterized by an elevated heart rate prior to surgery, can have a detrimental impact on patient outcomes. The exact incidence of perioperative tachycardia varies depending on factors such as the type of surgery, anesthetic techniques employed, and the patient's underlying medical conditions.
High heart rates can worsen hemodynamic instability, leading to complications such as hypotension, arrhythmias, and myocardial ischemia. Furthermore, perioperative tachycardia has been correlated with an increased risk of postoperative length of stay.
Recognizing the potential consequences, clinicians must actively monitor heart rate during the perioperative period and implement strategies to reduce tachycardia when required.
Tachycardia in the Operating Room: Assessment and Management
Tachycardia within the operating room can indicate a significant hemodynamic problem. A rapid heart rate demands prompt identification and suitable management to ensure patient safety.
The initial step involves a thorough comprehensive examination, including observing vital signs such heart rate, blood tension, and respiratory rate.
A detailed account of the patient's recent medical situation should furthermore be obtained to reveal potential underlying factors.
Heart monitoring is essential to confirm the form of tachycardia and detect any irregularities.
Diagnostic tests may be useful in determining electrolyte disruptions, thyroid status, and other elements that could be influencing to the tachycardia.
Based on the evaluation, management approaches should be tailored to the root cause and the patient's clinical condition.
Treatment options may include fluid infusion, sodium replacement, medication use to control heart rate and rhythm, and in some cases, emergent procedures such as synchronized cardioversion.
Continuous surveillance of the patient's vital signs and reaction to treatment is crucial throughout the perioperative period.
Factors Influencing Perioperative Heart Rate Dynamics
Perioperative heart rate dynamics are significantly influenced by a complex interplay of physiological factors. Preoperative patient characteristics such as age, preexisting medical conditions, and anxiety levels can contribute to baseline heart rate. Intraoperatively, anesthetic agents, surgical stimulation, and hemodynamic adjustments can alter heart rate. Postoperatively, pain, inflammation, and restitution also play a role in cardiac rhythm. Careful monitoring and intervention of these factors are crucial to ensure optimal cardiovascular outcomes during the perioperative period.
Post-Surgery Heart Rate Elevation
Post-operative tachycardia, characterized by an accelerated heart rate following surgery, can significantly/noticeably/potentially impact patient recovery. This condition can manifest as a result of various factors, including anesthesia, pain, and inflammation. While often temporary, persistent tachycardia may indicate/suggest/point to underlying complications, necessitating prompt/timely/immediate medical attention. Monitoring heart rate closely after surgery is crucial/essential/vital to ensure optimal healing and minimize potential risks associated with this common/frequent/usual postoperative phenomenon.
Perioperative Arrhythmias: Recognizing and Addressing Tachycardia
During the perioperative period, patients are at risk to developing arrhythmias. One of the most common types is tachycardia, characterized by a heart rate exceeding normal limits. Prompt recognition and management of tachycardia are essential to patient safety. Physiological signs can manifest as palpitations, shortness of breath, chest pain, dizziness, or fainting. Electrocardiography (ECG) is the fundamental tool for detecting tachycardia. Treatment methods depend on the underlying cause and severity of the arrhythmia. Drug therapy options include beta-blockers, calcium channel blockers, and antiarrhythmic agents.
In some cases, invasive procedures such as cardioversion or catheter ablation may be indicated.
Strategies for Minimizing Perioperative Tachycardia
Minimizing perioperative tachycardia requires a multifaceted approach that encompasses various pre-, intra-, and postoperative interventions.
A comprehensive evaluation of the patient's medical history, including underlying conditions and medications, is crucial for identifying potential risk factors contributing to tachycardia.
Preoperative optimization strategies such as judicious fluid management, electrolyte balance correction, and anxiolysis get more info can help mitigate autonomic activation.
During surgery, attenuating the hemodynamic stress response through careful anesthetic techniques, adequate analgesia, and temperature control is essential. Maintaining a calm and supportive environment for the patient can also contribute to reducing tachycardia.
Postoperatively, vigilant monitoring, early ambulation, and pain management are critical in facilitating regeneration and preventing post-operative complications.
Heart Rate Variability During Surgery: Insights into Cardiac Stress
During surgical procedures, patients often experience physiological stress. This can lead to alterations in various bodily functions, including heart rate variability (HRV). HRV, a measure of the fluctuation in time between consecutive heartbeats, provides valuable clues into the autonomic nervous system's activity. Reduced HRV during surgery has been linked with increased risk of complications.
Physicians and researchers utilize HRV monitoring as a potential tool to assess cardiac function during surgery. By analyzing the patterns of HRV, clinicians can gain a better knowledge of the patient's neurological state. This information can be instrumental in adjusting surgical strategies and ensuring optimal patient well-being.
- Additionally, HRV monitoring may serve as an early signal of impending cardiac concerns during surgery, allowing for timely treatment to mitigate potential risks.
- Nevertheless, the relationship between HRV and surgical stress is intertwined, requiring further investigation to fully elucidate its implications in clinical practice.
Anesthesia's Impact on Perioperative Tachycardia Management
Perioperative tachycardia presents a common challenge for anesthesiologists. Prompt and effective management is crucial to minimize adverse outcomes and ensure patient well-being. Anesthesiologists utilize a variety of techniques, including pharmacologic agents like calcium channel blockers, to regulate heart rate during both the induction and maintenance phases of anesthesia. Furthermore, optimizing anesthetic depth and monitoring hemodynamics closely are essential components of tachycardia mitigation. By implementing these strategies, anesthesiologists can effectively manage perioperative tachycardia and contribute to a successful surgical outcome.
Preoperative Risk Factors for Postoperative Tachycardia
Identifying individuals at risk for postoperative tachycardia is crucial for optimizing perioperative care. Several preoperative factors can contribute to this phenomenon. Increased age is a significant predictor, as the cardiovascular system may undergo greater stress during and after surgery. Pre-existing conditions such as hypertension, diabetes mellitus, and coronary artery disease can in addition elevate the likelihood of postoperative tachycardia. Additionally, certain anesthetic agents and surgical procedures themselves carry a risk for tachycardia.
- Preoperative medication use, particularly beta-blockers or anticholinergics, can also influence the risk of postoperative tachycardia. Individuals who are smokers may be more susceptible to this phenomenon due to nicotine's effects on heart rate and rhythm.
Early Detection and Intervention for Perioperative Tachycardia
Perioperative tachycardia, a common cardiovascular complication during surgical procedures, can have serious consequences for patient outcomes. Immediate detection and intervention are essential to reduce the risk of complications including myocardial ischemia, arrhythmias, and hemodynamic instability. Clinicians should employ a multi-pronged approach that involves continuous cardiac monitoring, meticulous intraoperative management, and timely pharmacological interventions. Additionally, patient education regarding surgical risk factors and strategies to optimize cardiovascular health can contribute to a safer surgical experience.
Optimizing Fluid Management to Prevent Tachycardia After Surgery
Maintaining hemodynamic stability after surgery is crucial for patient recovery. One key aspect of this management involves optimizing fluid administration to prevent tachycardia. substantial fluid shifts can trigger an elevation in heart rate, potentially leading to complications. Therefore, meticulous monitoring of fluid input and output is essential. A balanced approach, considering factors such as patient age, pre-operative status, and surgical procedure, will help clinicians ensure appropriate hydration levels. Close collaboration between the anesthesia team and the surgical team is crucial to implement a tailored fluid management strategy that minimizes the risk of postoperative tachycardia.
Perioperative Tachycardia: Influence on Surgical Outcomes
Perioperative tachycardia, a common physiological response during surgical procedures, has been shown to potential adverse outcomes. While some degree of tachycardia is normal in the perioperative period, prolonged elevations in heart rate can contribute various surgical issues. Studies have revealed a correlation between perioperative tachycardia and increased probability of postoperative complications such as wound infection, myocardial infarction, and prolonged hospital stay.
The underlying causes contributing to perioperative tachycardia are multifactorial and can include anesthetic agents, pain, stress, hypoxia, and autonomic nervous system imbalance. Identifying patients at greater risk for perioperative tachycardia is crucial for implementing appropriate interventions to mitigate its potential negative effects. Early identification and management of tachycardia can improve surgical outcomes, reduce postoperative morbidity, and enhance patient well-being.
Individualized Factors Influencing Postoperative Heart Rate
A multitude of individual factors can significantly influence postoperative heart rate. These factors encompass maturity level, preexisting medical conditions, and drug regimens the patient is receiving. Additionally, psychological elements such as nervousness can affect an elevated heart rate following surgery. Patients who are more active may exhibit a quicker recovery and therefore a quicker return to baseline heart rate. Conversely, patients possessing complications during or after surgery may experience a prolonged elevation in heart rate. Understanding these patient-specific factors is crucial for clinicians to assess postoperative heart rate and implement appropriate interventions to ensure optimal patient care.
Tachycardia Following Anesthesia
Tachycardia is/can be/presents as a common complication/occurrence/issue in the post anesthesia care unit recovery room. It refers to/describes/indicates a heart rate above/exceeding/greater than 100/120/140 beats per minute bpm. Several factors/A variety of etiologies/Multiple contributors can contribute/lead to/cause tachycardia in the PACU, including/such as/among which are residual anesthetic effects, pain, anxiety, dehydration, hypovolemia, and electrolyte imbalances/disruptions/disturbances. Early identification/Prompt recognition/Detecting tachycardia is crucial/essential/important to ensure/guarantee/facilitate patient safety. Clinicians should/must/are required to monitor heart rate closely and implement/utilize/apply appropriate interventions such as/including/in cases of fluid resuscitation, medications, and addressing underlying causes/factors/origins.
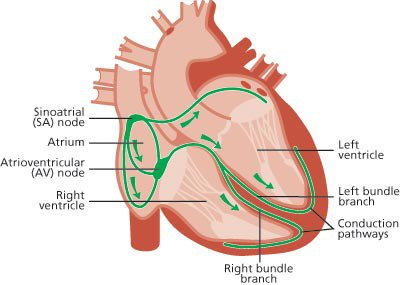
The Autonomic Nervous System and Perioperative Tachycardia
Perioperative tachycardia, a common occurrence during surgical procedures, stems from the interplay between the sympathetic and parasympathetic divisions of the autonomic nervous system. These branches dynamically regulate physiological processes to maintain homeostasis. During surgery, various factors such as anesthesia administration, surgical stimuli, and emotional stress can precipitate sympathetic activation, leading to an acceleration in heart rate. Conversely, parasympathetic activity may diminish, contributing to the overall tachycardia. Understanding this complex interplay is crucial for effective perioperative management and minimizing adverse outcomes.
Strategies for Perioperative Tachycardia Detection
Effective management of tachycardia during the perioperative period demands meticulous monitoring strategies. Clinicians employ a variety of techniques to detect elevated heart rates, which can signify underlying issues.
Continuous electrocardiogram (ECG) assessment provides real-time visualization of cardiac rhythm and rate. Heart rate monitoring can also detect tachycardia by measuring pulse rate alongside oxygen saturation levels. Invasive hemodynamic parameters, such as arterial blood pressure and central venous pressure, can provide additional insights about the cardiovascular condition.
Prompt detection of tachycardia allows for timely treatments to restore heart rate and prevent potentially critical complications.
Report this page